1/6/2021
·Enable high contrast reading
What Do Parents Value Regarding Pediatric Palliative and Hospice Care in the Home Setting?

Summary of survey results published in the Journal of Pain and Symptom Management
Jackelyn Y. Boyden, PhD, MPH, RN; Mary Ersek, PhD, RN, FPCN; Janet A. Deatrick, PhD, RN, FAAN; Kimberley Widger, PhD, RN, CHPCN(C); Gwenn LaRagione, BSN, RN, CCM, CHPPN; Blyth Lord, EdM; Chris Feudtner, MD, PhD, MPH
Introduction
Courageous Parents Network is proud to work with provider-researchers who are investigating issues and questions common to the lived experience of families caring for very sick children. This study, published in the July 2020 Journal of Pain and Symptom Management, is an inquiry into what pediatric palliative care services (PPC) families caring for children at home most value. For the study, the investigators recruited CPN and other families in the U.S. to better understand how they prioritize a wide range of palliative and hospice services. This is a non-technical description of the study and results. For more in-depth information, read the published article.
The study
More and more children with life-limiting illness and complex care needs are being cared for by their families at home, particularly toward end of life. They and their families are supported by a range of palliative and hospice services and providers. Because the resources are limited, or finite, it is important for the medical community, advocates and government agencies to effectively allocate what is available. Understanding what the primary caregivers, mainly families, value should be an important factor in guiding these decisions. Families’ values can also be an indicator of where care needs improvement.
A team of researchers set out to investigate family priorities in a recent study of parents recruited from the Children’s Hospital of Philadelphia (CHOP) Pediatric Advanced Care Team (PACT), as well as from Courageous Parents Network (CPN), using the CPN newsletter and social media to invite participation. All of those who responded were screened and provided electronic informed consent. They completed a survey via a Web link, either together with the researchers or independently. Participants were compensated with a gift card for their time and effort.
The families
Forty-seven parents from 45 families participated in the study. Most participants were mothers, who were white, non-Hispanic, married or partnered, and had completed college or graduate school. About one-third (30%) of participants were bereaved and many (70.2%) were caring for their child at home during the study. 34% received care for their child from CHOP; the other 66% were CPN families who received care from providers across the United States.
The participants were parents to 45 children who have received pediatric palliative care. Approximately half of the children were 0-9 years, and half were 10-25 years. The most prevalent diagnoses included neuromuscular, neurologic, or mitochondrial (51.1%), genetic or congenital (48.9%), cardiovascular (22.2%), and metabolic (22.2%) diseases.
Study design
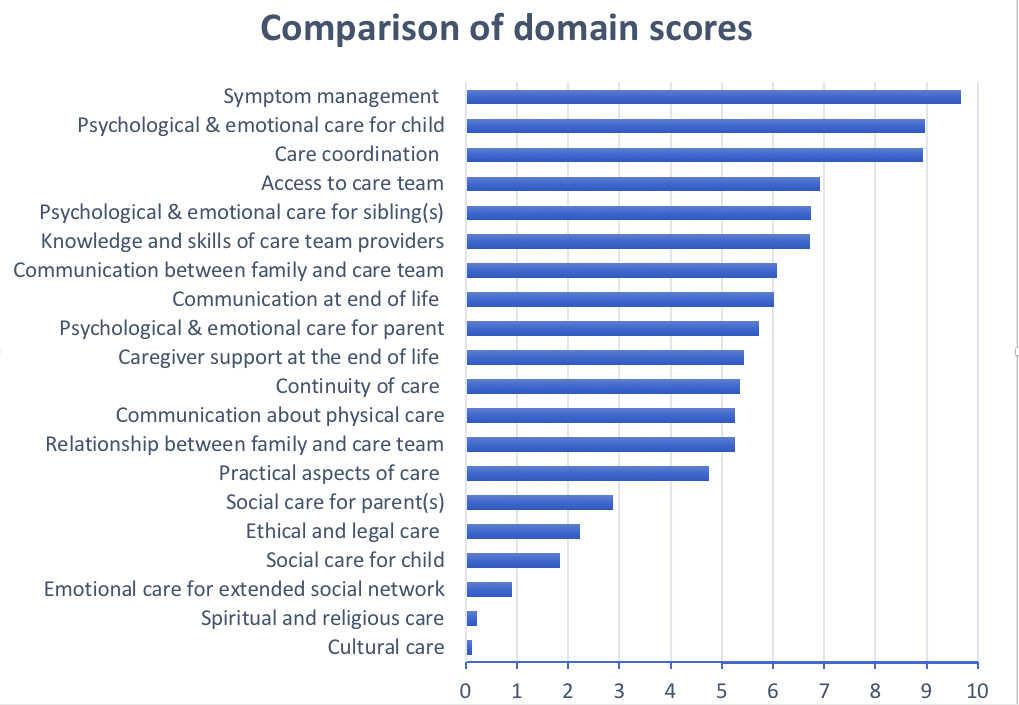
The participants received a list of 20 “domains,” or features, of high-quality pediatric palliative and hospice care in the home. This list covered a wide range of services provided by PPC and hospice providers. All participants were given definitions of the domains to ensure that everyone surveyed had the same understanding of what was intended. They were presented with different combinations of the 20 domains; each time, they were given 4 domains and asked to choose the domain that they felt was the most important in supporting their child in the home, and the one they felt was least important. Then, using statistical analysis, the researchers calculated scores for each of the domains. The domains were then placed on a scale, from most important to least important, to represent how the domains ranked (or compared) in importance to each other. For example, a domain with a score of 10 was considered by participants as twice as important as a domain with a score of 5. The full list of domains and their definitions is included in the article.
Results
Parents ranked the domains Symptom management the highest, followed by Psychological & emotional aspects of care for the child, and Care coordination. Among the lowest-ranked domains were Emotional care for the family’s extended social network, Spiritual and religious care, and Cultural care.
The results differed somewhat based on different groups of families. For example, parents with other children rated the domain Psychological & emotional care for the sibling(s) as a higher priority, and in fact twice as important, than did families without other children. Bereaved parents rated the Caregiver support at the end of life domain as more important than did families currently caring for their child, and not necessarily facing end-of-life issues. There were no significant differences between the scores of the 44 mothers and the three fathers who participated in the study.
Conclusion
In their report, they also noted four limitations of the study:
- The demographic characteristics of the participants were relatively similar. Additional research with larger and more diverse samples is recommended, so that we can more fully understand parental priorities, particularly among underrepresented groups.
- The study did not collect data on the actual programs families receive or that are available. As a result, parents may have evaluated a domain as less important if the services addressing the domain were ineffective or unavailable, or if families chose not to use them.
- Although the domains were based on NCP Guidelines for Quality Palliative Care and informed by PPC-specific guidelines and a panel of PPC stakeholders, the study may have left out important domains.
- The study does not address how much the rankings might change over time for families; for this, studies that follow families over time are needed.
Nevertheless, the researchers believe that these results present important directional feedback for future conversations about prioritizing finite resources and focusing care improvement efforts.
This infographic is another way to read the findings: PediatricPalliativeatHome_Study_Infographic_2021-01-05
Thank you
Many thanks to the CPN parents who participated in this study! If you are interested in contributing your knowledge and experience to future efforts, please watch your CPN newsletter and be certain to follow CPN on Facebook and LinkedIn.
Additional Note
The researchers are currently working on developing a questionnaire to help measure how families experience these domains of palliative and hospice care at home. The goal of this questionnaire is for families to provide real-time (that is, at the time they are receiving care) feedback to their providers, so providers can work together with families to make sure that the care they receive is meeting their needs. The first phase of this development project included the same CPN and CHOP families mentioned in the summary above, who also helped prioritize items to include on this questionnaire (published article coming soon).
In the second phase of this project, beginning in January 2021, they will be working with families currently caring for their children at home, as well as with palliative care and hospice providers, on making this questionnaire more useful for families and for providers. If you are interested in helping out with this next project, please keep an eye on our CPN newsletter and social media pages for more details that will be coming out soon. This is how we families make it better for those that follow.