-

A diagnosis of Krabbe; and the medical t...
-

We were so caught up in having a new bab...
-

Adding Hospice to the Care Team
-

What does a “good day” look like? Em...
-

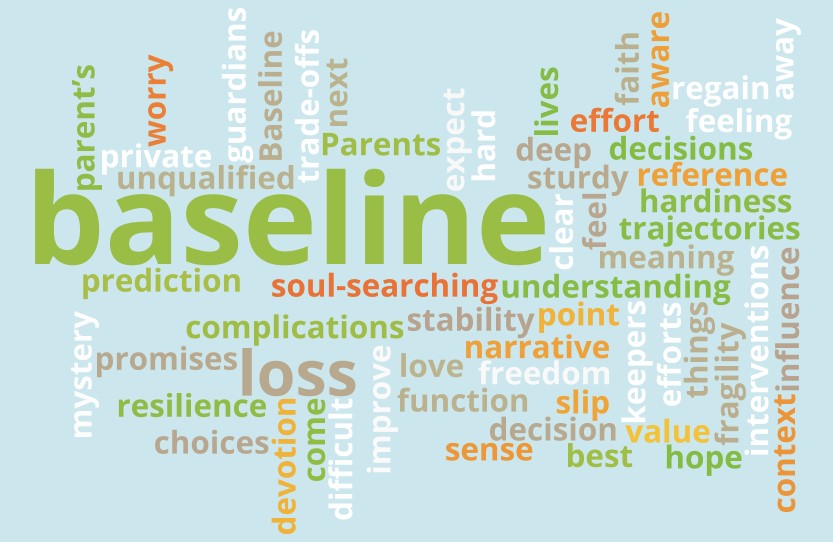
This is How We Live: This Thing Called B...
-
Problems of the CNS: Is this a new acute...
-
Intractable problems and a new Baseline:...
-
The Conversation and Advance Care Planni...
-

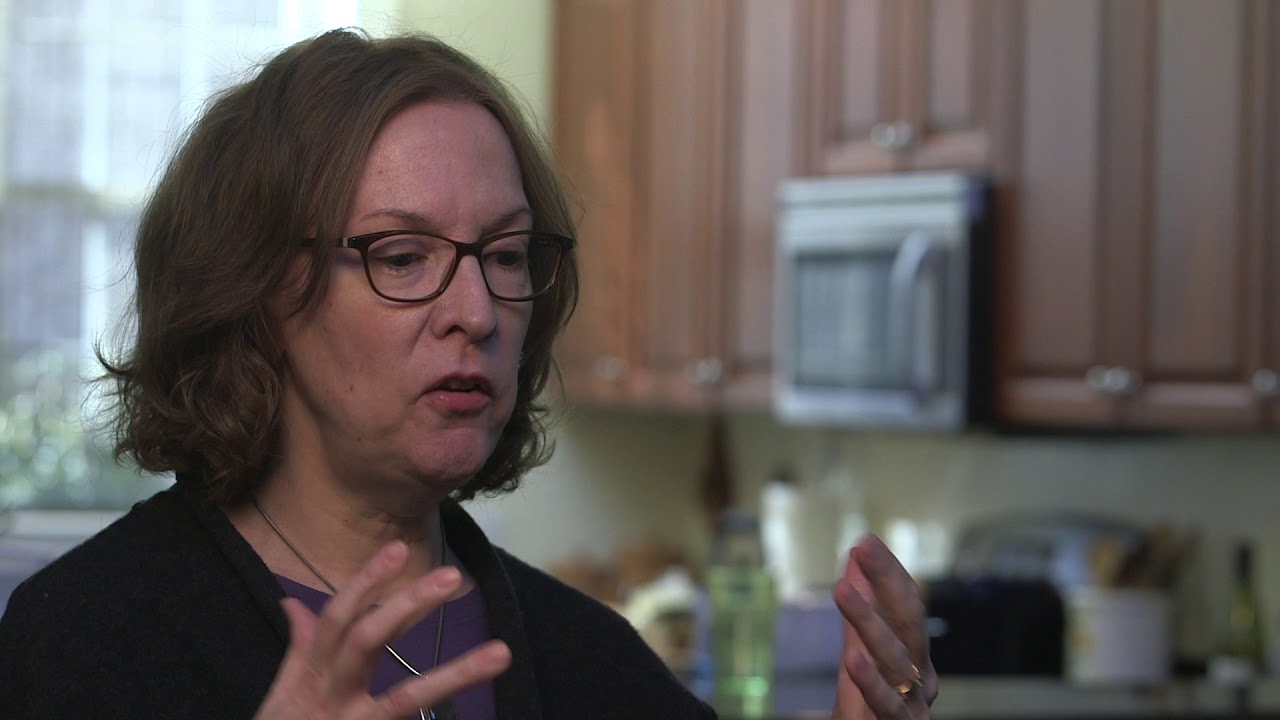
Palliative care helps parents pause and ...
-

Always give them a sense of what’s goi...
Videos
Theme: Baseline
A diagnosis of Krabbe; and the medical team getting to meet him before his condition progressed.

A diagnosis of Krabbe; and the medical team getting to meet him before his condition progressed.
SHARE