Dysautonomia and Hypothermia
The autonomic nervous system (ANS) regulates normal function in the body, such as heartbeat, blood flow, breathing, body temperature, bowel and bladder control, sleep/wake cycles and digestion, without our awareness. Dysautonomia in children with SNI is caused by signaling problems in the areas of the brain that control these autonomic functions. Dysautonomia can present in different ways, and sometimes it occurs without a trigger or can be caused by a temporary problem, such as an infection.
Your Team:
An interdisciplinary specialist who helps manage the medical, social and emotional challenges of complex and/or long-term care.
A specialist in the management and treatment of neurological conditions, or problems with the nervous system.
A specialist whose aim is to improve the quality of life of their patients over the course of their illness regardless of stage, by relieving pain and other symptoms of that illness.
A medical specialist in rehabilitation with the goal of restoring and enhancing functional ability and improving quality of life. See Orthotist
A medical professional who practices general medicine.
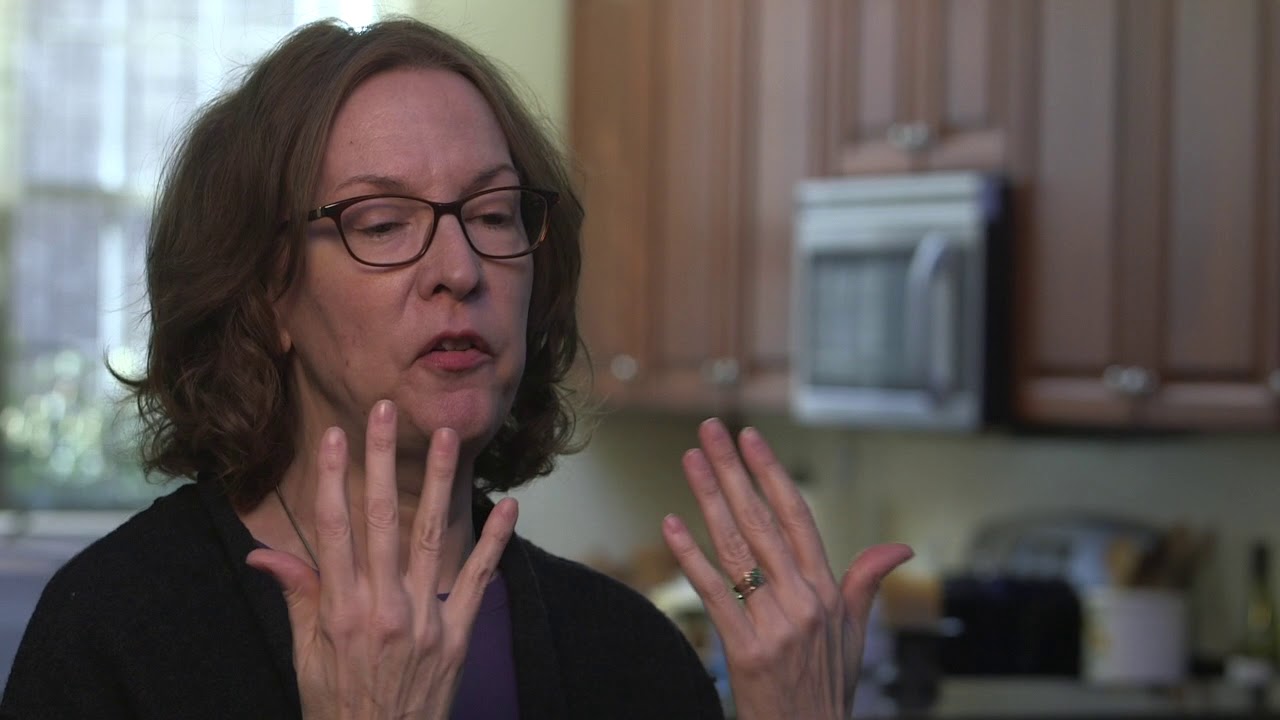
Your child’s primary physician and complex care clinicians can assess for problems that can look like or trigger dysautonomia. A neurologist and physical medicine and rehabilitation specialist can provide input on how brain function may be impacting symptoms and, in some cases, recommend medications to improve the symptoms. Complex care and palliative care clinicians can coordinate between specialists and help guide care goals.
Dysautonomia
Autonomic dysfunction can cause these changes to happen suddenly and intermittently.
Quiet Features
Active Features
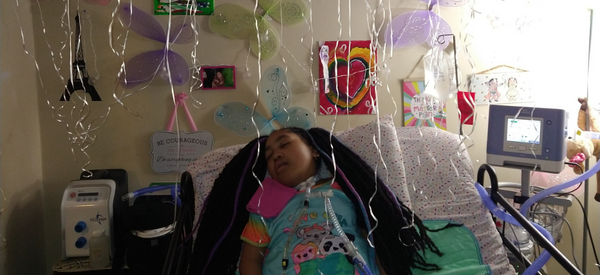
Acute events with active features are often referred to as autonomic storms. During a storm your child may appear to be in pain, feel warm or sweaty, have red skin, experience an increase in muscle tightness, and/or display tremors or jerking limbs. The heart rate and blood pressure, if measured, will usually be elevated. An event that persists can be due to a new problem, like an acute infection. Sometimes a trigger, like a need for personal care and repositioning or overstimulation, can be identified. Other times triggers cannot be identified, and the storms are hard to predict. The medical team can help develop a plan to manage these events.
Treatment of activated autonomic dysfunction includes scheduled or daily medications. Like chronic neuropathic pain, treatment can decrease but not prevent all episodes. Autonomic storms are often treated by adding a medication to the management plan on an as-needed basis. Effective treatment will also include identifying and treating other problems, such as constipation, spasticity and/or other causes of pain, which can trigger and activate the ANS.
Hypothermia
Children with SNI may also experience hypothermia, or low body temperature. Hypothermia is defined as a body temperature below 95° F (35° C). Some children with SNI have recurrent drops in their body temperature. This is because the body’s core temperature is regulated by the hypothalamus, a part of the brain that connects the endocrine and nervous systems. When your child’s nervous system is compromised they may be at risk for hypothermia. However, hypothermia may also be a sign of infection or could occur without a clear trigger.
Chronically low body temperature is manageable. Experiment with blankets, hat and scarf, heating pad (not placed directly on the skin, and for no more than one hour at a time) and increasing room temperature. Your child’s body temperature will slowly increase with these interventions, but it can take a while–six to eight hours–for the temperature to increase to 95° F (35° C).
Take and record your child’s temperature twice a day for a week to develop a sense of what is their “normal.” Certain body systems don’t work as effectively at lower temperatures, so it is important to talk with your medical team if your child’s body temperature is consistently low. And, if at any time your child’s health baseline changes, or if you and your child’s clinicians are seeing new neurological decline, repeat the process. Keep up to date records in your child’s care plan. This will help the clinicians evaluate whether a temperature change is part of your child’s new baseline, or is a symptom of another issue (for example, an infection) that should be addressed.
 English
English
 العربية
العربية
 Français
Français
 Español
Español