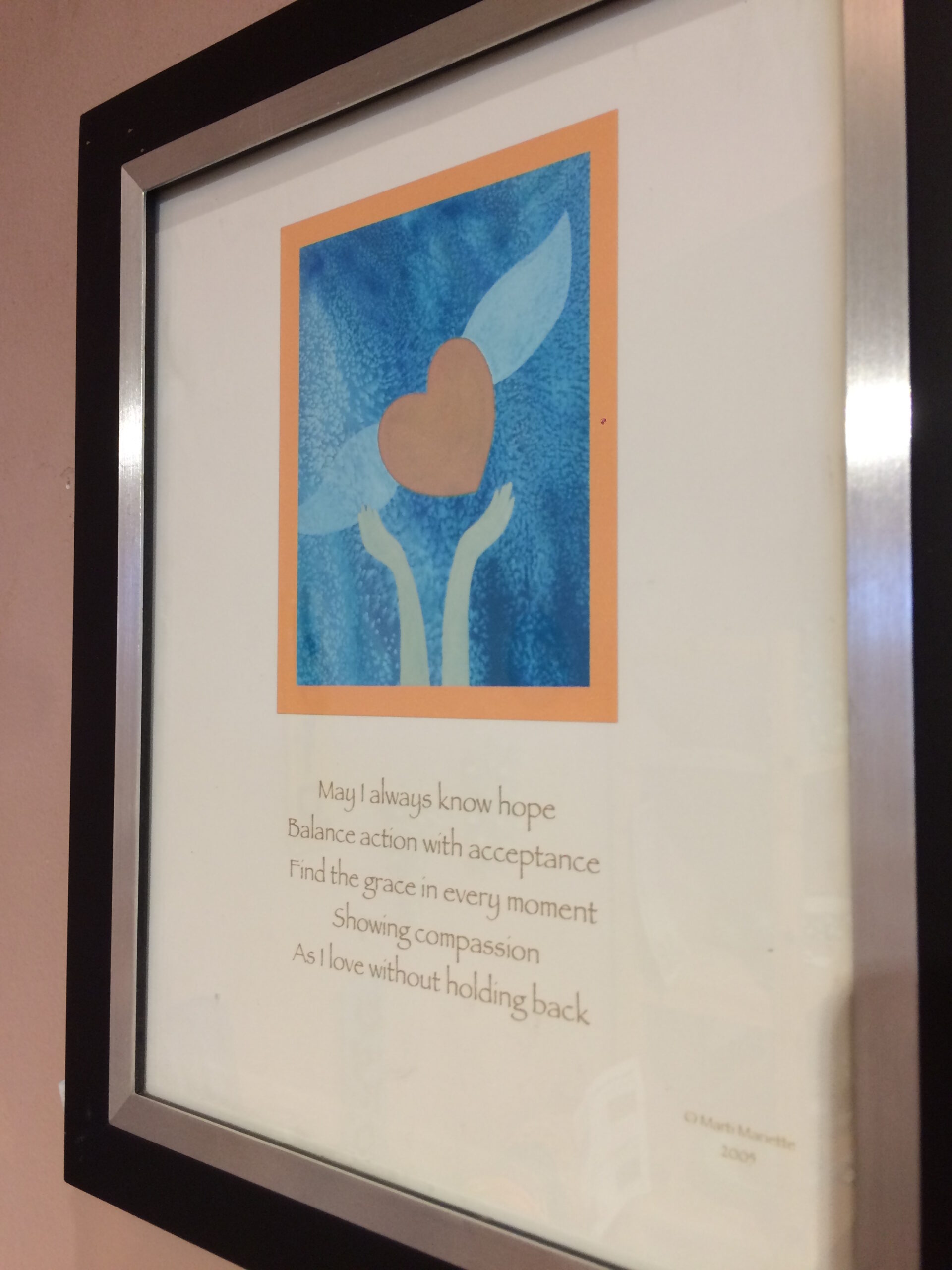
When my son was just over one month old, my husband and I went on a date. It was a rainy November day in 2016, and we were determined to leave the house together to do something, anything, not related to baby duty. Of course, as a new mom whose infant son had just spent a harrowing week at the local children’s hospital and been diagnosed with mitochondrial disease, it was hard to tear myself away. But, in our visit to a local art studio, I found a piece of inspiration that informed my parenting journey profoundly, and helped me embrace palliative care early in my son’s life. A beautiful drawing of a pair of hands, lifting up a heart with wings, and a quote:
“May I always know hope
Balance action with acceptance
Find the grace in every moment
Showing compassion
As I love without holding back”
This simple poem, prayer, koan became my mission statement for living a purposeful and peaceful life with my son. For feeling, in some small way, that I could shape the gutting actuality of his disease into an exuberant existence. I’d like to say that when his neurologist first recommended that my husband and I meet with our hospital’s Pediatric Advanced Care Team (PACT), I immediately tapped into these guiding words and scheduled that meeting with a smile on my face. Of course, that’s not what happened, but this idea of balancing “action with acceptance” helped me get to that place much sooner than I may otherwise have.
My son’s neurologist recommended we pursue conversations about palliative care when, at about seven months old, my son’s seizures had not come under control of medication despite multiple attempts. I immediately bristled at the suggestion to meet with the PACT, and sharply asked “Aren’t those the people who help with things like advanced directives?” I was in raging denial that we might need to deal with something like that, so soon in our son’s life. The doctor gently explained that yes, advanced directives are included in the PACT scope of work, but so were many other things related to helping our son live a comfortable life, and helping us as parents feel in control of our decisions related to his care. I cannot overstate how powerful it was to have a doctor explain her palliative care referral in a way that positioned it as an opportunity for influence, rather than a form of resignation.
Since that time, my husband and I have met with the Pediatric Advanced Care Team twice. The first time, when our son was about eight months old, was a simple “get to know you” conversation. We were able to share more about our son’s incredible personality, his primary diagnosis, his constellation of symptoms, and our hopes, fears, and values for our family. The PACT representatives explained the many ways they could help us, such as accompanying us to clinic visits, facilitating complex decisions about our son’s care with us and his army of medical providers, serving as a sounding board for me and my husband, or making referrals to outside community agencies for respite or other support. I realized the important differentiating factor between them and our son’s doctors: our son’s doctors are (rightly) focused on the physical manifestations of his disease. The palliative care providers help us focus on all the other ways those manifestations impact his, and our, lives – in our heads, in our hearts, in our home.
Our second meeting was more recently, just this past December, as we prepared for our son’s G-tube surgery. My husband and I both felt strongly that placing a G-tube was the right thing to do, but we wanted to be on the same page about why we felt that way. So, we went to our meeting with the PACT armed with the following discussion topics (and influenced by the CPN Framework for Difficult Decisions):
- Why does this intervention feel appropriate at this time? Under what circumstances would we stop using this intervention?
- Assuming all things remain the same – what would happen if we stopped using his G-tube and his ‘failure to thrive’ went untreated?
- What are other potential interventions or medical decisions that we might need to consider in the future? How do we feel about them currently?
As a result of this conversation, my husband and I came away with some insights into the value of palliative care that I hope may be useful for others considering incorporating it into their child’s life.
- For us, palliative care is not a plan. It’s a philosophy. There are far too many medical and developmental variables related to our son’s condition for us to do any concrete scenario planning. But, by naming our priorities and our uncertainties with the PACT, we can co-create mutual understanding that ultimately serves our son. The PACT learns about our family’s values and priorities, while my husband and I learn about caretaking options we may not otherwise have been aware of. In our most recent discussion, we learned more about what comfort feeding is. We also learned about some medical circumstances where short term vs. long term invasive interventions may be relevant, and were in a safe space to talk about our feelings related to that.
- Perhaps most critically, palliative care providers help families hold an incredibly intricate space. When your child has a life-limiting illness, there are no easy conversations about their futures, and there are no right answers. Every situation is deeply unique. These are not issues we want to discuss with family and friends, largely because they are private, but also because we want loved ones to be able to engage with our son, not his disease. We have been fortunate that, thus far in our son’s life, we have not had to make any quick decisions about his care, nor have we had to make decisions under extreme emotional duress. But the possibility is always there. Understanding that there are people on our team who know us, and him, and can reflect our priorities back to us in challenging or exhausting times is a huge source of comfort.
I was a nervous wreck prior to our son’s G-tube surgery, but on the actual day, I found myself full of calm. In that beautiful space between action and acceptance. I knew we had thought through our decision as fully as possible. This allowed me to release lingering feelings of anxiety and self-recrimination, and be fully present for my son during his recent procedure and current recovery. This capacity for presence, aided by palliative care, is invaluable to me as a mom, who, fifteen months into my son’s life, marvels at his beauty, strength, and potential every single day.
________________________________________________________________________________________________________________
Liz Morris loves exploring complex questions. Her professional experiences in project management, librarianship, and community development prepared her well for her favorite role as mom to Colson. Colson, impacted by mitochondrial disease since birth, inspired Liz to face the complicated aspects of his life through writing and advocacy. Liz serves as a family advisor at Seattle Children’s Hospital, and is a volunteer ambassador for the United Mitochondrial Disease Foundation. She is committed to helping families find the information they need to help them live well in the face of life-limiting illness. You can find Liz on Instagram @mrsliz.morris