Neonatal Intensive Care
The NICU is unlike any other environment and can feel strange and disorienting. This is not how you had hoped for your child’s life to begin, and you are understandably worried for their future. The medical team is compassionate and understanding, but the rules are strict. Things may change at any time; decisions must be made. You are focused on your vulnerable child but aware that others need you—and you need them too. The NICU may be very overwhelming, but recognizing what you’re feeling can make your stay seem a little more manageable.

Your Team:
A member of the clergy who is responsible for the religious needs of an organization and/or its constituents.
A specialist whose aim is to improve the quality of life of their patients over the course of their illness regardless of stage, by relieving pain and other symptoms of that illness.
A mental health professional who uses therapy and other strategies to support coping and adjustment and treat concerns regarding social, emotional, or behavioral functioning.
A trained professional who works with people, groups and communities to help them better their lives.
A professional who teaches lessons about emotions, thoughts, coping skills, facing fears, and more.
Neonatologists are pediatric clinicians specially trained in caring for sick and premature infants. A psychologist, therapist, or chaplain or other advisor can offer emotional and spiritual support. Palliative care clinicians can help you clarify your goals for your child and act as a liaison with the other medical team members. A social worker also offers this support and can help with other basic care needs for you and your family.
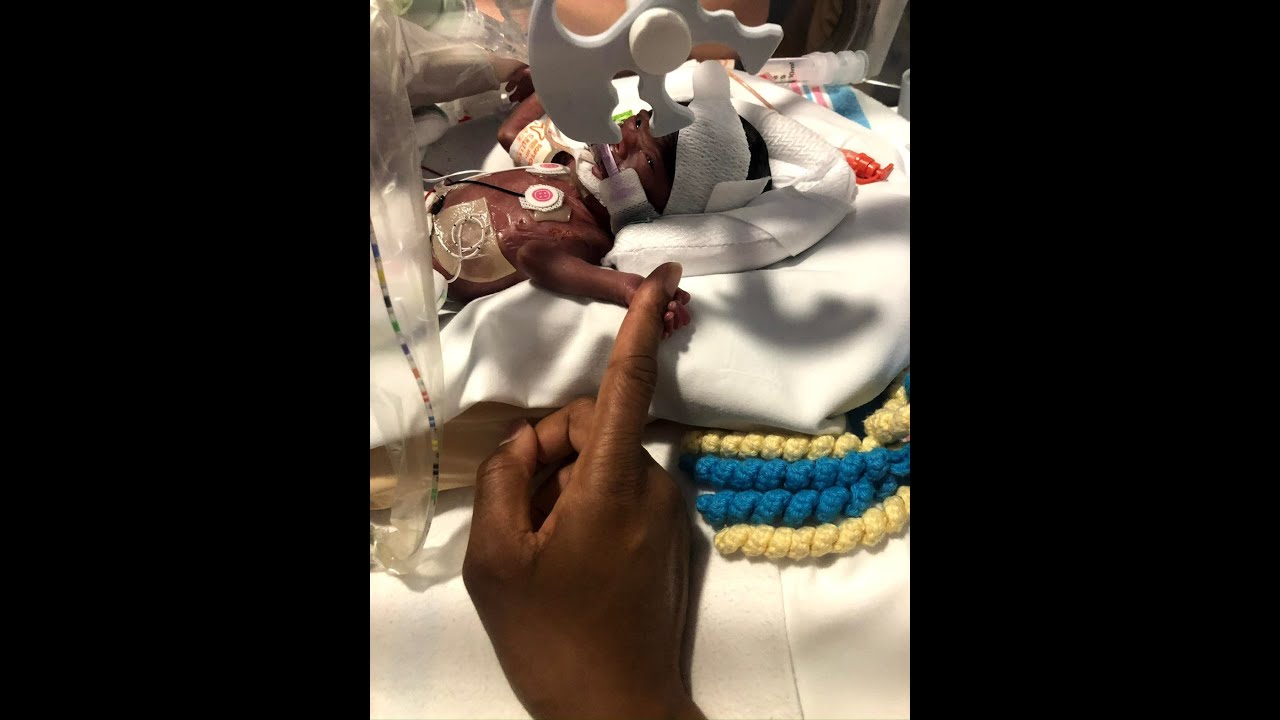
Your child needs you in other ways too. In many situations you can be together at almost all times. Once your baby is stable you will be encouraged to hold them. Physical contact, especially skin to skin, helps you and the baby bond—to feel mutual love and security. The NICU will teach you other ways to care for your newborn as well, depending on their condition and needs.
It’s no wonder that emotions are high and strong. At the same time that you may wish to be happy and excited, it is perfectly normal to be anxious and upset. You may be frightened for your child and fearful for their future and for your family. You may be angry and/or have feelings of guilt. You and your co-parent, if you have one, may have feelings about getting close to the baby. You may have different reactions at different times, and your feelings may change at any given time. In fact, you may find moments of joy and hope as you come to know your child and this new reality.
It is important during this stressful time to take care of yourself as much as possible. It may be hard to leave your child, even for a moment, but spend just a few minutes away from the NICU each day. Check in with family and friends when you can, to take in their love and support. And try to sleep and eat well. As with everything else that is ahead, you will be better able to cope when you are feeling strong and rested.
Exploring your feelings with a professional can be very helpful. You might also find support from other parents who have experienced life in the NICU. Ask what support groups and counseling are available to you. The section Orienting to Hospital includes useful information to help you adapt. The CPN guide “Framework for Sharing Decision-Making with Your Child’s Clinicians” can also be a helpful resource.
– Frances M., clinician
Related Resources
-
 A mother on learning she needed to take care of herself while her baby was in the NICU.video
A mother on learning she needed to take care of herself while her baby was in the NICU.video -
 Finding HOME in the NICU and the HeartBLOG
Finding HOME in the NICU and the HeartBLOG -
 Deciding which parent stays in the NICU.video
Deciding which parent stays in the NICU.video -
 A Letter to Myself, One Year AgoBLOG
A Letter to Myself, One Year AgoBLOG -
 Parents give tips on being in the NICU: Staying present, creating routines, holding your child as is possible; pumpingvideo
Parents give tips on being in the NICU: Staying present, creating routines, holding your child as is possible; pumpingvideo -
 Medical Uncertainty: What the data says vs. what is going to happen with this particular baby.video
Medical Uncertainty: What the data says vs. what is going to happen with this particular baby.video -
 Decision-making in the NICU: When the mom and dad are thinking at different scales of timevideo
Decision-making in the NICU: When the mom and dad are thinking at different scales of timevideo -
 "I did not get it right every day, and I'm still learning to give myself grace with the process "video
"I did not get it right every day, and I'm still learning to give myself grace with the process "video