Siblings at End of Life
Whether or not they have been told directly, children often have a sense that their sibling’s health is seriously declining. As much as any adult, they will likely anticipate end of life in their own age-related way, have questions and concerns, and need support.
Your Team:
A member of the clergy who is responsible for the religious needs of an organization and/or its constituents.
A mental health professional who specializes in bereavement and loss.
A person who gives help and advice to students about educational and personal decisions.
A person trained to care for the sick, especially in a hospital.
A specialist whose aim is to improve the quality of life of their patients over the course of their illness regardless of stage, by relieving pain and other symptoms of that illness.
A medical professional who practices general medicine.
A mental health professional who uses therapy and other strategies to support coping and adjustment and treat concerns regarding social, emotional, or behavioral functioning.
A trained professional who works with people, groups and communities to help them better their lives.
An individual who leads and/or guides individuals or groups coping with life experience and challenges.
An educator.
A psychologist, social worker, chaplain and/or spiritual leader can provide a safe space for siblings to talk and share their emotions. A grief counselor can help process strong emotions. Palliative care clinicians and child-life specialists can offer age-appropriate ways of talking with siblings and facilitate special moments and memory-making. Your child’s primary physician can offer a deeper understanding of the family. A school nurse, guidance counselor, or teacher can provide support.
It may feel unthinkable to openly talk about the changes that are occurring in your dying child, and to talk about death. It can be especially hard to know how to bring siblings into this conversation, especially if the changes are very sudden or are occurring very rapidly. Know that speaking honestly and gently can offer comfort and help reassure your children that the family unit will survive this very difficult time and tremendous loss. In being open with them, you will create a foundation of support, space and trust to talk about difficult things, now and in the future.
As with most things, it is helpful to learn about what siblings already know, have heard, are thinking. This conversation can provide a jumping-off point to share new information, explore questions and worries, and clarify any misunderstanding. You may find yourself having to answer many difficult and painful questions, some of which you may not have answers for. Be honest and direct, using age-appropriate language. Words like death and dying help avoid confusion, as many other terms (e.g., passing on, departing) are vague and have multiple meanings. This is particularly true for young children, who tend to be concrete thinkers and take things quite literally.
In these and all conversations, keeping a developmental frame in mind will help you speak to, and respond to, sibling questions, worries, fears and other concerns.
- Infants have no cognitive understanding of death, but they do grieve. They may experience death as separation, and often sense a caregiver’s emotional state, so it is important to maintain routines and avoid separation when possible.
- Preschool children (ages 2-5) see death as temporary and reversible, as in cartoons. Magical thinking (around age 5) is characteristic, and so preschoolers may believe that a death is the result of something they did or didn’t do, or that they somehow have the power to cause the death (or reverse it).
- Children ages 6-9 are concrete thinkers but still do not understand that death is permanent. They still may believe that it will never happen to them or anyone they know.
- Children ages 9-11 remain concrete thinkers. They have some capacity to put themselves in other people’s shoes and may have a sense that others can die.
- Around age 12, children begin to have abstract thinking and come to understand that death is final, irreversible, and will happen to everyone. Adolescence, however, has many phases and each phase may bring with it different responses.
– Jenn, parent of Mallory
Supporting Siblings’ Reactions and Feelings
It is extremely helpful to make others in the siblings’ community—especially teachers, friends’ parents, and, if relevant, their faith community—aware of what is happening at home. This will prepare them to anticipate and understand changes in behavior such as sudden tears, anger, other acting out or asking direct questions about life and death. Let other adults know how you are responding so that they can be consistent and supportive.
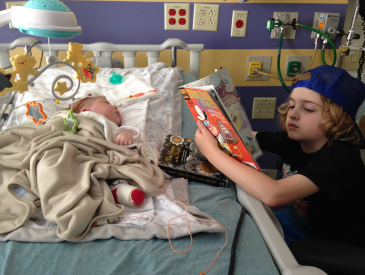
Involving Siblings
Whether siblings should be present at the death is a big question for many parents. Speaking to a member of the care team, a pediatric psychologist or therapist, a close relative, or someone who knows the siblings, can help you decide what is best for your family. You might consider other options, like encouraging your other children to make or give something special to the dying sibling as they say goodbye. There is no right or wrong answer.
Related Resources
-
 Siblings: Holding on to hope while also understanding death may happen. “The staff was worried she was too hopeful, unrealistic.”video
Siblings: Holding on to hope while also understanding death may happen. “The staff was worried she was too hopeful, unrealistic.”video -
 A pediatric palliative care social worker on involving the siblings at End of Life.video
A pediatric palliative care social worker on involving the siblings at End of Life.video -
 Communicating with the siblings: What can we do to make this as less traumatic as possible, to minimize damage.video
Communicating with the siblings: What can we do to make this as less traumatic as possible, to minimize damage.video -
 Siblings: “I wracked my brain about how to make his last days better.”video
Siblings: “I wracked my brain about how to make his last days better.”video -
 IN THE ROOM: What Siblings Wantevent
IN THE ROOM: What Siblings Wantevent