How an Instruction in Critical Care Became a Philosophy of Living
The room is dim except for the flickering of the pulse oximeter’s slow waveform. My hands are on her small body, rolling her onto one side. Even this simple act requires choreography: lift under the shoulder, steady at the hip, watch the feeding tube, the oxygen, the monitor cords that twist like roots if you’re careless. She exhales with a wet rattle that tells me which lung needs help. I listen, adjust the pillow under her ribs, and tilt her until the rhythm evens.
“Good lung down.”
I wrote good lung down in the notebook and now the words arrive before the memory does. A respiratory therapist said them once, many admissions ago, while angling her in the hospital bed just so. I can still see his hand on the rail, the confidence of habit. “You want the healthy lung on the dependent side,” he said, “so it can carry the weight, help the other expand.” He spoke like it was obvious. At the time, it wasn’t.
Now it is.
Her right lung was the good one that night, the left still recovering from pneumonia. Her body was warm and surprisingly heavy. Not dead weight, but dense with sleep and medication. I kept a hand against her ribs, feeling for the subtle lift that means air is reaching where it couldn’t before. Gravity does its slow work. I’ve done this hundreds of times, but it never becomes autopilot. Each turn asks for precision. Her body’s healing depends on such small degrees.
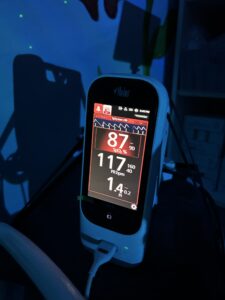
When her breathing steadies, I step back. The pulse-ox climbs: eighty-seven, then ninety-three. I exhale with her. Between each breath the room seemed to hold its own too. The phrase hums in my head like a refrain, less instruction now than ritual. The waiting that follows is its own form of care.
 There was a night, early on, when I got it backwards. She’d been restless for hours, her numbers dipping, and I thought I could make her more comfortable by turning her away from the sore side. Within minutes the monitor shrieked. I remember the panic, the scramble to correct, the instant relief when I put her good lung down again, the breath returning. I learned that lesson in the blunt language of oxygen saturation.
There was a night, early on, when I got it backwards. She’d been restless for hours, her numbers dipping, and I thought I could make her more comfortable by turning her away from the sore side. Within minutes the monitor shrieked. I remember the panic, the scramble to correct, the instant relief when I put her good lung down again, the breath returning. I learned that lesson in the blunt language of oxygen saturation.
The body doesn’t lie about imbalance.
Still, I kept living by the wrong orientation in my own quiet ways. When people asked how we were doing, I gave the wins: a stable week, a smile, a rare stretch of sleep. I performed competence habitually and protectively, the way you perform posture. I didn’t want to burden anyone with the other side of it, the fatigue that seeps into bone, the private griefs that have no clear edge. I led with the good lung up, trying to keep what hurt from showing.
That’s what most of us do. We present the stable side first, compressing the rest beneath it. We tell ourselves it’s for others’ comfort, or our own control. But over time the pressure builds; the wounded parts can’t expand. Somewhere in those long hospital nights, I began to wonder if I’d been positioning myself backwards. I’d been protecting the hurt instead of giving it air. I’d been tucking it away, the way you’d cradle a wound and tell yourself it’s safer that way. But the physics didn’t work. Healing required exposure, dependence, gravity. The good lung had to go down so the bad could breathe again.
What if the same logic applied beyond the body?
She’s resting now, angled just right, her chest lifting in a steady rhythm. The good lung down, bearing the weight so the other can open. The physics of healing is counterintuitive. But the lungs know what the mind resists: expansion requires exposure.
other can open. The physics of healing is counterintuitive. But the lungs know what the mind resists: expansion requires exposure.
I think about that often, the physics of healing. How the stronger side becomes foundation, not façade. How what is whole steadies what is struggling. We’re taught a different pattern, of course: stay positive, be strong, keep the hurt tucked away. Especially in the world of care the performance of lone resilience becomes reflex. Strangers call you amazing. Providers say you’re an inspiration. You start to confuse endurance with enlightenment. You mistake competence with completeness.
But that’s bad lung down.
When we lead with where we are strong by ignoring where we are weak, we smother the places still trying to breathe. We compress the grief until it can’t clear, the exhaustion until it ferments into shame. “Good lung down” suggests letting stability carry the pressure so fragility can have air. The good doesn’t disappear; it simply takes a supportive role.
This integration is essential when dealing with loss that has no clear boundary; what some call ambiguous loss. The life I grieve is a ghost that coexists with the life I have. I cannot bury this grief, nor can I cut it out; the body is here, but the expected future is gone. The work is not to achieve closure, but to achieve meaning-making by allowing the healthy parts of my identity and my life to bear the weight of the reality, not to deny it, so that the wounded parts (the fatigue, the fear) can be positioned for true expansion. The fragile side must be seen and supported, not suppressed.
This isn’t wallowing, you aren’t sanctifying the bad lung. But this also isn’t extirpation, you don’t cut out the affected lung. You reposition it and allow the wounded parts to face the air, trusting the rest of you to hold steady. Healing isn’t heroic, it’s gravitational. It’s the slow rotation toward openness, the willingness to let pain expand instead of sealing it off.
Like respiratory care, it’s a practice. You listen, adjust, wait. You keep turning until the breath moves freely again. There’s tenderness in that discipline. The same precision I use for her body belongs elsewhere too. To my own heart, to the unseen spaces that tighten when I try too hard to protect them. The wisdom is already there: the strong must be yielding for the fragile to heal.
True healing comes not from hiding but from bringing the hurt to light and allowing stronger parts to hold. Which means that true strength comes from being supportive, not from dominating.
Good lung down. Not forever. Just long enough.
What, or who, are the ‘good lungs’ in your life? Who are you the ‘good lung’ for? Are you letting them hold your hurt? Are you holding theirs?
If you would like to share your response to Bud’s question in an email please send to connect@courageousparentsnetwork.org and we will be sure Bud receives it.
 Stephen Hager goes by his second middle name (he has three), Bud, because it’s easier to remember and baristas never misspell it. Along with his wife he is a caregiver for their 8-year-old daughter, Emma, who has pachygyria, a rare neurological disorder. He believes in taking an active approach to advocating for his child and others like her. To this end, he sits on various advisory councils at Children Hospital of Orange County (CHOC), volunteers on consulting and directing boards for various non-profit centers and lends his writing skills where he can. Experiencing a lack of support for parents of medically complex children, Bud founded a support group through CHOC focusing on parent-to-parent interaction. He is also a professor of psychology and has a small private psychotherapy practice.
Stephen Hager goes by his second middle name (he has three), Bud, because it’s easier to remember and baristas never misspell it. Along with his wife he is a caregiver for their 8-year-old daughter, Emma, who has pachygyria, a rare neurological disorder. He believes in taking an active approach to advocating for his child and others like her. To this end, he sits on various advisory councils at Children Hospital of Orange County (CHOC), volunteers on consulting and directing boards for various non-profit centers and lends his writing skills where he can. Experiencing a lack of support for parents of medically complex children, Bud founded a support group through CHOC focusing on parent-to-parent interaction. He is also a professor of psychology and has a small private psychotherapy practice.
